The Significance of Governing Healthcare Apparatus
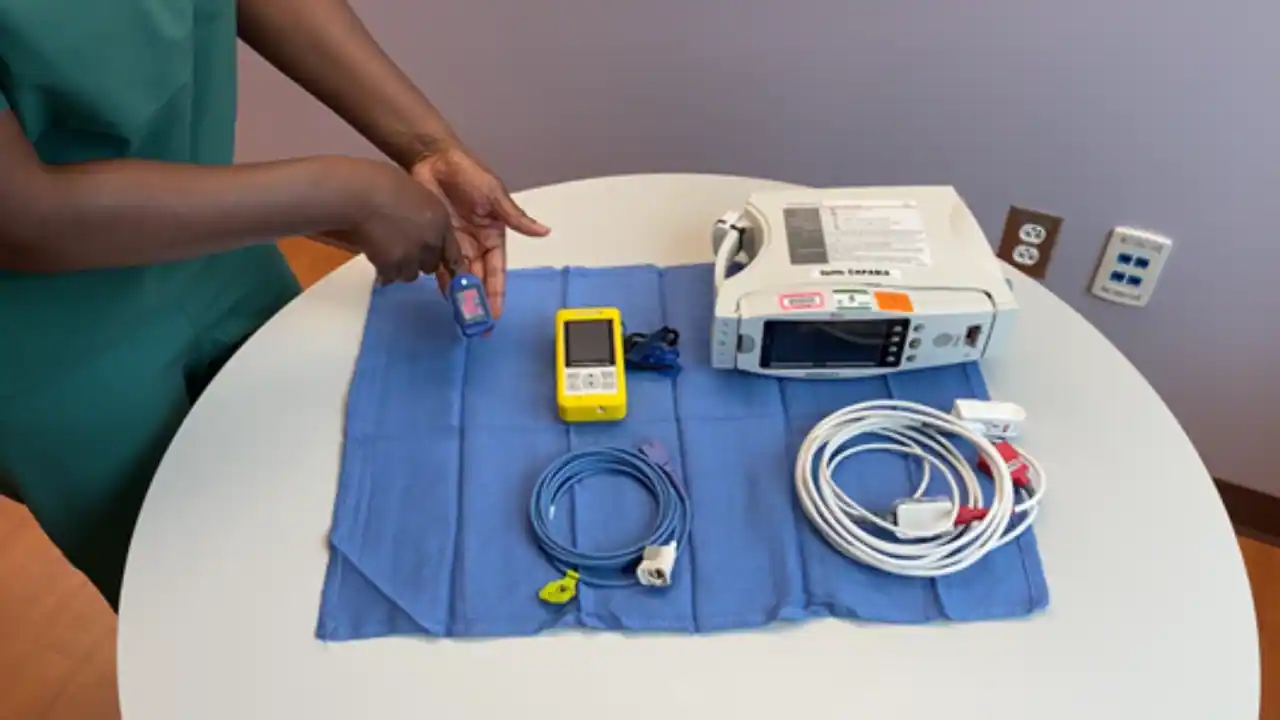
Healthcare Instruments
“A healthcare instrument can encompass any tool, device, tool, equipment, apparatus, implant, substance for in vitro application, software, substance, or other akin or correlated item, designed by the creator to be utilized, alone or collectively, for a healthcare intention.”
With a surplus of two million healthcare instruments in existence currently, representing myriad categories, the necessity to guarantee their dependability, security, and affordability is unmistakable.
Healthcare instruments are essentially the products of engineers, contrasting with pharmaceuticals originating from the work of chemical specialists. Furthermore, the market audience for each of these products varies significantly, along with the associated risks and the methodologies utilized to assess the efficiency and efficacy of the specific item.
Healthcare instruments span a spectrum from infusion pumps and drug-eluting stents to implants and cardiac pacemakers.
Development of Regulation for Healthcare Instruments
Possibly the earliest iteration of control over healthcare instruments involved a straightforward examination and testing of medical apparatus manufactured by UK industries in a rapid takeover from international producers during the war, due to the impracticality of continued imports in that circumstance. However, as healthcare instruments gained momentum, becoming increasingly sophisticated and widely accessible, the recognition of the necessity for manufacturing and product standards emerged, leading to the recruitment of specialists.
This gave rise to the establishment of a comprehensive regulatory system and a post-market surveillance strategy. A voluntary quality assurance system was also instituted to enhance design and production. Additionally, inspections were introduced to ensure adherence. Subsequently, formal assessment programs for healthcare instruments were implemented. Later on, unified statutory systems were established for the entire European Union.
An analogous regulatory supervision is exercised in the United States by the Food and Drugs Administration (FDA). Numerous regulatory authorities adopt a tiered approach based on the level of risk associated with each usage and the potential for user and manufacturer error. This is because the highest level of regulation is neither necessary nor feasible for the least risky category of healthcare instruments.
Why Govern Healthcare Instruments?
Healthcare instruments aid in diagnosing, treating, or monitoring individuals with potential disease conditions. To accomplish this, they must fulfill their intended purpose, be durable, and avoid harm to the patient and operator. Several studies have highlighted that with the global marketing of healthcare instruments, an increasing number of adverse events are being reported, including severe and fatal incidents.
Indeed, within a decade in the USA, with its stringent and extensive regulatory system, there have been well over 1.5 million injuries and over 80,000 deaths. A notable instance of poorly regulated healthcare instruments was the aggressive promotion of vaginal mesh, resulting in severe pain, bleeding, and other serious side effects following its application in vaginopexy. Despite being introduced in 2002, it took nearly two decades for the FDA to retract its approval.
Regulation aims to ensure that healthcare instruments become safer, of superior quality, and possess better designs. Naturally, regulation involves increased costs for manufacturers concerning development, production processes, and services. This will elevate prices for healthcare providers and patients, constraining device sales and impeding innovation.
Despite this argument, several compelling reasons advocate for the regulatory supervision of healthcare instruments. Numerous cases, such as the aforementioned vaginal mesh incident, have been reported globally, indicating that healthcare instruments have often been inadequately regulated, resulting in harm and fatalities for patients.
Dr. Thimbleby articulated some fundamental points in his thought-provoking essay. Initially, he highlights that patients are the focal point of healthcare and should always be central to all technology utilized in healthcare. Secondly, technology aims to make things more compact, lighter, and cheaper to produce, thereby increasing profitability; the goal is never to make people well.
Thirdly, human nature remains unaltered despite the rapid evolution of technology. People still desire authority, those in power pretend to be infallible, and nobody likes to accept blame. Finally, technology is ceaselessly evolving. Before one solution is entirely developed, someone is likely to have an even better idea – rendering the previous one obsolete and potentially necessitating the abandonment of the former, but at the potential cost of losing data or skills.
These facts elucidate the necessity for regulation of healthcare instruments.
Safety
Healthcare instruments should not cause harm to those who use or operate them. Instead, they should improve the well-being of the patient. Adherence to healthcare instrument regulations is crucial to demonstrate the veracity of this claim. Instruments like implants and cardiac pacemakers, which are likely to present a higher safety risk, undergo more stringent regulation than others, such as contact lenses and adhesive plasters.
Standardized Requirements
By standardizing the fundamental design and prerequisites, it is feasible to ensure that all products introduced for a healthcare purpose meet these prerequisites. Standards for other facets may be developed, but these are met voluntarily. Any technology may be employed, as long as the process and final product align with the essential requirements.
Instrument development, design, and clinical studies are part of the checkpoint framework and quality control and production procedures. Post-marketing, users are encouraged to report adverse events, and the manufacturer is obliged to report serious adverse events. This facilitates the identification of safety issues for corrective action.
Encouraging Innovation
In addition to keeping non-compliant products off the market, regulatory supervision can redirect the focus towards genuinely beneficial changes, such as safer, more effective, or more economical instruments – either individually or in combination. Indigenous product development will also be incentivized, for both domestic and international sales, if regulations in the manufacturing country align with those of the exporting nations.
Facilitating Goods Movement
Uniform standards enable the import and export of goods without necessitating independent studies between countries. Transparency regarding instrument compliance with regulatory standards and pricing regulation is also ensured, providing fair market access and clinical safety, thereby improving product selection.
Recompense
Stringent regulation enables patients to receive compensation for harm caused by instrument defects.
Exploring New Areas
“The rigor of the approval process for higher-risk products, which might only require bench-testing data and possibly some clinical study, and the delay in responding to new findings about adverse events have been repeatedly questioned.”
Nurturing Innovation
Innovative or personalized healthcare instruments are often developed based on previously approved instruments, so that, theoretically, the new instrument is a variation of the older one. The newer ones may fall outside the realm of approval, becoming unregulated. This ongoing conflict between innovation and regulation is vital for patient safety and benefit.
At times, regulatory criteria impede innovation, as meeting the standards may be too costly and time-consuming. Conversely, standards may sometimes be inadequate to provide proper evaluation criteria.
For instance, providing open-source designs for commonly used healthcare instruments allows others to freely enhance the design, share their innovations, and offer rapid end-user feedback. However, this also interferes with regulation and quality control.
With a limited number of units, documentation for regulatory approval may be excessively expensive. On the other hand, the prescribed steps for development and testing may be forsaken for non-traditional processes like 3D printing. Hence, regulatory systems must be rigorous enough to protect the patient but flexible enough to accommodate novel approaches that foster innovation.
One instance is the necessity for shared and updated documentation, preventing the duplication of development and testing efforts for the same part, tracking the original design, the underlying design process, the rationale behind it, and subsequent changes.
Logical Testing
Another area of consideration is the requirement for testing based on the real-world utilization of the instrument rather than in optimal laboratory conditions. This is because the latter fails to replicate the instrument’s actual performance during operational conditions by individuals with varying levels of training and operating under diverse circumstances.
Widespread utilization instruments should ideally undergo testing in a broader context, considering their application beyond typical clinical settings.
In numerous instances, health applications also circumvent regulatory criteria, where self-verification is deemed sufficient.
Combination products of drugs and devices are presently in development, subject to pharmaceutical regulation and, independently, to medical device regulation in instances of uncertainty regarding whether the product falls under pharmaceutical or medical device categorization. Aside from this, the degree of regulation ensuring a higher level of consumer safety is applied.
Conclusion
For enhanced regulation of healthcare instruments, all involved parties should engage in the process, encompassing the industry, researchers, patients, and payers. Real-world data should be utilized to make informed decisions.
“For medical technology, standards and regulations are necessary to ensure security, safeguard the public, and ensure that products are suitable for their intended use. However, in the context of innovative and personalized medical technologies, the current approach to regulation is not only impractical and challenging to enforce but also operates against healthcare innovation. Regulators may need to reconsider their approach.”
On the flip side, it holds true that “Future technological advancement is poised to continuously transform healthcare, yet while technologies (novel drugs and treatments, innovative instruments, novel social media support for healthcare, etc.) will steer innovation, human factors will persist as one of the enduring limitations of breakthroughs.”
Source: https://www.news-medical.net/
References:
- Jefferys, D. B. (2001). The regulation of medical devices and the role of the Medical Devices Agency. British Journal of Clinical Pharmacology. https://dx.doi.org/10.1046%2Fj.0306-5251.2001.01416.x. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2014554/
- Public Health: Stronger Rules on Medical Devices (2021). https://ec.europa.eu/commission/presscorner/detail/en/ip_21_2617
- Ung, C. O. L. (2019). Should Medical Devices Be Regulated as Rigorously as Drugs? Canadian Journal of Hospital Pharmacy. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6799957/
- Shah, A. R. et al. (2008). Current Status of the Regulation for Medical Devices. Indian Journal of Pharmaceutical Sciences. https://dx.doi.org/10.4103%2F0250-474X.49085. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3040860/
- Regulation of Medical Devices: A Step-By-Step Guide. https://apps.who.int/iris/handle/10665/249571
- Vincent, C. J. et al. (2015). Can Standards and Regulations Keep Up with Health Technology? JMIR mHealth and uHealth. https://doi.org/10.2196/mhealth.3918. https://mhealth.jmir.org/2015/2/e64/
Thimble by, H. (2013). Technology and the Future of Healthcare. Journal of Public Health and Research. https://dx.doi.org/10.4081%2Fjphr.2013.e28. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4147743/
Further Resource:
- BladGo: Your Convenient On-the-Go Bladder Scanne
- https://bladgo.com/